Volume 29, Issue 2 (Spring 2023)
Intern Med Today 2023, 29(2): 105-115 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shahrokhi H, Fallah Mohammadi M, Naderi A, Nabizadeh Z. Effects of Core Stabilization on Lumbopelvic Motor Control and Pain in Patients with Nonspecific Chronic Low Back Pain: A Randomized Clinical Trial. Intern Med Today 2023; 29 (2) :105-115
URL: http://imtj.gmu.ac.ir/article-1-4016-en.html
URL: http://imtj.gmu.ac.ir/article-1-4016-en.html
1- Department of Sports Pathology and Corrective Movements, Faculty of Sports Sciences, Hakim Sabzevari University, Sabzevar, Iran. , h.shahrokhi@hsu.ac.ir
2- Department of Sports Sciences, School of Humanities, Shafagh Institute of Higher Education, Mazandaran, Iran.
3- Department of Health and Exercise Sciences, School of Sport Sciences, Shahrood University of Technology, Shahrood, Semnan, Iran.
2- Department of Sports Sciences, School of Humanities, Shafagh Institute of Higher Education, Mazandaran, Iran.
3- Department of Health and Exercise Sciences, School of Sport Sciences, Shahrood University of Technology, Shahrood, Semnan, Iran.
Full-Text [PDF 1351 kb]
(744 Downloads)
| Abstract (HTML) (2080 Views)
.png)
![]()
Figure 1. Flowchart of subject recruitment and allocation
![]()
Figure 3. Swiss ball exercise program
Table 2. Group means of experimental and control groups at pre-test, post-test, and follow-up for pain and motor control
Table 3. Summary of independent t-test results
Table 4. Summary of the repeated-measures ANOVA and the Bonferroni posthoc test results for pain and motor control in pre-test, post-test, and follow-up
Full-Text: (440 Views)
Introduction
Low back pain (LBP) is a common musculoskeletal disorder experienced by 70%-80% of people in their lifetime [1]. Approximately 5%-10% of patients develop chronic back pain, leading to high healthcare costs, productivity loss, and individual disability [2]. LBP is a major contributor to global disability and ranks sixth in overall burden [3]. Often nonspecific, LBP lacks a specific underlying cause but can lead to various complications, such as increased trunk force variability, body stiffness, and reduced movement variability in the lower limbs.[4, 5]. These complications contribute to impaired trunk muscle control, increased oscillation of the center of pressure and mass, changes in body position, decreased nerve conduction velocity, and increased thigh and trunk movements [6]. In addition, the condition can be worsened by disuse atrophy and decreased muscle strength [7].
The economic burden of LBP is substantial, with annual direct costs ranging from €2.3 billion to €2.6 billion and indirect costs between €0.24 billion and $8.15 billion in high-income countries. The pooled annual hospitalization rate for LBP is 3.2%, with per-patient direct costs averaging USD 9,231 and total costs around USD 10,143. These figures underscore the extensive financial impact of LBP, highlighting the need for effective management and prevention strategies[8].
Evidence-based research has demonstrated that therapeutic exercise is a widely recommended and effective treatment for LBP, either on its own or in combination with other therapies [9, 10, 11]. In recent years, there has been a growing recognition of the significance of core stability due to studies indicating that patients with LBP experience delayed or reduced activation of specific muscles, leading to a compromised support system for the lumbar spine and an increased burden on its joints and ligaments, potentially resulting in more stress and strain [12]. Core stabilization exercises have been recognized for their positive impact on the strength, endurance, and flexibility of spine muscles, as well as their ability to train stabilizing muscles involved in movement, promoting control and stability in the lower back [13]. Moreover, core stabilization exercises improve the feed-forward mechanism during peripheral limb movements, thereby ensuring lumbopelvic motor control and stability [4]. Nevertheless, there is ongoing debate regarding whether core exercises are more effective than general exercise for lower back pain [14, 15].
It is crucial to have a thorough understanding of the potential benefits of core stabilization exercises for chronic nonspecific lower back pain [16]. One common type of recommended exercise involves unstable surfaces, although specific reasons and the overall effectiveness of this approach remain unclear. Some studies have been conducted in this field so far. For instance, Young et al. (2015) compared the effectiveness of proprioceptive neuromuscular facilitation integration patterns and Swiss ball training on balance and pain in elderly patients with chronic low back pain[17]. The researchers reported that the proprioceptive neuromuscular facilitation integration pattern was superior to Swiss ball exercises in the improvement of balance; nonetheless, they found no significant differences in functional tests and pain intensity results [17].
Given the close link between pain and motor control in LBP patients, it seems helpful to assess the effect of core exercise on both of these variables[18]. Yet, this effect is not well-studied among patients with chronic nonspecific LBP[19]. Motor re-education is of utmost importance in addressing the causes of LBP, specifically alterations in muscle recruitment patterns and impaired trunk muscle movement[20]. Core exercises on a Swiss ball have been demonstrated to induce neuroplastic changes in the nervous system, leading to improved muscle activity and trunk muscle recruitment for spinal stabilization[21, 22]. Furthermore, it has been revealed that exercising on Swiss balls is enjoyable and motivating for individuals[20, 23]. Given the significant impact of chronic LBP on motor control, core stabilization using a Swiss ball could be a beneficial training approach for enhancing motor control and reducing pain in these patients [20, 23].
Research in the field of Swiss ball core stabilization exercises for chronic nonspecific LBP is essential due to the significant prevalence and impact of LBP globally, ranking as the sixth leading cause of disability[2]. Chronic LBP not only imposes a substantial economic burden but also results in individual disability and decreased quality of life[3, 24]. Despite the availability of various treatment options, there remains a need for effective strategies to address the complexities of LBP, including impaired trunk muscle control and increased body stiffness[1]. The present research sought to bridge the existing gaps by explicitly investigating the efficacy of Swiss ball exercises in alleviating pain and improving motor control in patients with chronic nonspecific LBP. An improved understanding of these interventions enables us to potentially enhance patient outcomes, reduce healthcare costs, and alleviate the overall burden of LBP on individuals and society.
The present study aimed to assess the impact of Swiss ball core stabilization on the amount of pain and motor control in the lumbar region of patients with chronic nonspecific LBP and its persistence in a one-month follow-up.
Low back pain (LBP) is a common musculoskeletal disorder experienced by 70%-80% of people in their lifetime [1]. Approximately 5%-10% of patients develop chronic back pain, leading to high healthcare costs, productivity loss, and individual disability [2]. LBP is a major contributor to global disability and ranks sixth in overall burden [3]. Often nonspecific, LBP lacks a specific underlying cause but can lead to various complications, such as increased trunk force variability, body stiffness, and reduced movement variability in the lower limbs.[4, 5]. These complications contribute to impaired trunk muscle control, increased oscillation of the center of pressure and mass, changes in body position, decreased nerve conduction velocity, and increased thigh and trunk movements [6]. In addition, the condition can be worsened by disuse atrophy and decreased muscle strength [7].
The economic burden of LBP is substantial, with annual direct costs ranging from €2.3 billion to €2.6 billion and indirect costs between €0.24 billion and $8.15 billion in high-income countries. The pooled annual hospitalization rate for LBP is 3.2%, with per-patient direct costs averaging USD 9,231 and total costs around USD 10,143. These figures underscore the extensive financial impact of LBP, highlighting the need for effective management and prevention strategies[8].
Evidence-based research has demonstrated that therapeutic exercise is a widely recommended and effective treatment for LBP, either on its own or in combination with other therapies [9, 10, 11]. In recent years, there has been a growing recognition of the significance of core stability due to studies indicating that patients with LBP experience delayed or reduced activation of specific muscles, leading to a compromised support system for the lumbar spine and an increased burden on its joints and ligaments, potentially resulting in more stress and strain [12]. Core stabilization exercises have been recognized for their positive impact on the strength, endurance, and flexibility of spine muscles, as well as their ability to train stabilizing muscles involved in movement, promoting control and stability in the lower back [13]. Moreover, core stabilization exercises improve the feed-forward mechanism during peripheral limb movements, thereby ensuring lumbopelvic motor control and stability [4]. Nevertheless, there is ongoing debate regarding whether core exercises are more effective than general exercise for lower back pain [14, 15].
It is crucial to have a thorough understanding of the potential benefits of core stabilization exercises for chronic nonspecific lower back pain [16]. One common type of recommended exercise involves unstable surfaces, although specific reasons and the overall effectiveness of this approach remain unclear. Some studies have been conducted in this field so far. For instance, Young et al. (2015) compared the effectiveness of proprioceptive neuromuscular facilitation integration patterns and Swiss ball training on balance and pain in elderly patients with chronic low back pain[17]. The researchers reported that the proprioceptive neuromuscular facilitation integration pattern was superior to Swiss ball exercises in the improvement of balance; nonetheless, they found no significant differences in functional tests and pain intensity results [17].
Given the close link between pain and motor control in LBP patients, it seems helpful to assess the effect of core exercise on both of these variables[18]. Yet, this effect is not well-studied among patients with chronic nonspecific LBP[19]. Motor re-education is of utmost importance in addressing the causes of LBP, specifically alterations in muscle recruitment patterns and impaired trunk muscle movement[20]. Core exercises on a Swiss ball have been demonstrated to induce neuroplastic changes in the nervous system, leading to improved muscle activity and trunk muscle recruitment for spinal stabilization[21, 22]. Furthermore, it has been revealed that exercising on Swiss balls is enjoyable and motivating for individuals[20, 23]. Given the significant impact of chronic LBP on motor control, core stabilization using a Swiss ball could be a beneficial training approach for enhancing motor control and reducing pain in these patients [20, 23].
Research in the field of Swiss ball core stabilization exercises for chronic nonspecific LBP is essential due to the significant prevalence and impact of LBP globally, ranking as the sixth leading cause of disability[2]. Chronic LBP not only imposes a substantial economic burden but also results in individual disability and decreased quality of life[3, 24]. Despite the availability of various treatment options, there remains a need for effective strategies to address the complexities of LBP, including impaired trunk muscle control and increased body stiffness[1]. The present research sought to bridge the existing gaps by explicitly investigating the efficacy of Swiss ball exercises in alleviating pain and improving motor control in patients with chronic nonspecific LBP. An improved understanding of these interventions enables us to potentially enhance patient outcomes, reduce healthcare costs, and alleviate the overall burden of LBP on individuals and society.
The present study aimed to assess the impact of Swiss ball core stabilization on the amount of pain and motor control in the lumbar region of patients with chronic nonspecific LBP and its persistence in a one-month follow-up.
Materials and Methods
Study design and participants
This randomized clinical trial (IRCT20200107046035N5) employed pre-test, post-test, and follow-up assessments. The study included 24 participants with nonspecific chronic LBP, comprising 12 females and 12 males, with a mean age of 42.08±7.05 years. G*Power3.1 software was utilized to determine a sample size of 12 participants in each group for the study, considering an effect size (d) of 0.50 based on a previous study[25], significance level (α) two-tailed set at .05, and a desired power (1-β) of .80.
The inclusion criteria entailed participants aged 30-50 with chronic nonspecific LBP lasting at least three months and an Oswestry Disability Index above 16%. These individuals were required to be referred to an orthopedist. On the other hand, the exclusion criteria were as follows: acute LBP, spinal stenosis or surgery, inflammatory disease affecting the spine, fracture, spondylolysis or spondylolisthesis, use of relevant medication, symptoms associated with specific LBP lumbopelvic surgery, lower limb, and abdominal surgery in the past three months, and prior core stability training or athletic experience[24]. This study obtained approval from the Institution Review Board (IR.SSRC.REC.1399.076), and all participants provided informed consent.
Randomization
Participants meeting inclusion criteria were enrolled by an independent and blinded researcher. Random allocation to the experimental or control group was determined by a computer-generated sequence, employing a block size of 2, 4, 6, and an allocation ratio of 1:1. Group assignments were concealed in sealed envelopes opened after participants completed baseline assessments. Participants were randomly assigned to the experimental or control group (block size of 2, 4, 6 allocation ratio 1:1), as depicted in Figure 1. Demographic information was collected, and data were gathered before and after six weeks of core stability exercises for the training group, with a one-month follow-up. A laboratory specialist, not directly involved in the study and blinded to the interventions, performed the clinical assessments. The data analysts were blinded to group allocation. Participants were instructed not to reveal or discuss treatment with the evaluator.
This randomized clinical trial (IRCT20200107046035N5) employed pre-test, post-test, and follow-up assessments. The study included 24 participants with nonspecific chronic LBP, comprising 12 females and 12 males, with a mean age of 42.08±7.05 years. G*Power3.1 software was utilized to determine a sample size of 12 participants in each group for the study, considering an effect size (d) of 0.50 based on a previous study[25], significance level (α) two-tailed set at .05, and a desired power (1-β) of .80.
The inclusion criteria entailed participants aged 30-50 with chronic nonspecific LBP lasting at least three months and an Oswestry Disability Index above 16%. These individuals were required to be referred to an orthopedist. On the other hand, the exclusion criteria were as follows: acute LBP, spinal stenosis or surgery, inflammatory disease affecting the spine, fracture, spondylolysis or spondylolisthesis, use of relevant medication, symptoms associated with specific LBP lumbopelvic surgery, lower limb, and abdominal surgery in the past three months, and prior core stability training or athletic experience[24]. This study obtained approval from the Institution Review Board (IR.SSRC.REC.1399.076), and all participants provided informed consent.
Randomization
Participants meeting inclusion criteria were enrolled by an independent and blinded researcher. Random allocation to the experimental or control group was determined by a computer-generated sequence, employing a block size of 2, 4, 6, and an allocation ratio of 1:1. Group assignments were concealed in sealed envelopes opened after participants completed baseline assessments. Participants were randomly assigned to the experimental or control group (block size of 2, 4, 6 allocation ratio 1:1), as depicted in Figure 1. Demographic information was collected, and data were gathered before and after six weeks of core stability exercises for the training group, with a one-month follow-up. A laboratory specialist, not directly involved in the study and blinded to the interventions, performed the clinical assessments. The data analysts were blinded to group allocation. Participants were instructed not to reveal or discuss treatment with the evaluator.
.png)
Figure 1. Flowchart of subject recruitment and allocation
Outcome measures
Measurements were taken at three time points: baseline, the end of a six-week intervention, and after one month of follow-up. The primary outcome measured was pain intensity using a visual analog scale (VAS) ranging from 0-10. Secondary outcomes included lumbopelvic motor control, which was assessed using various tests, such as the knee lift abdominal test, bent knee fall-out test, waiter's bow test, sitting knee extension test, and transversus abdominis test. Acceptable reliability is demonstrated for this test battery[26, 27]. Further details about these outcome measures are presented in Table 1.
Pain Measurement: VAS measures the pain of patients subjectively. This scale is a 10-centimeter line, and patients are asked to grade their pain condition from 0 (no pain) to 10 (extreme amount of pain). The validity and reliability of this instrument have been reported to be very high [28].
Lumbopelvic Motor Control Measurement: The following tests were administered to assess lumbopelvic motor control, ensuring no order effects by randomization and incorporating one-minute breaks between each test. Participants completed three familiarization trials before each test.
Knee lifts abdominal test: The participant was lying on their back with their arms at their sides and feet on the floor. They were administered a test by gently raising their leg while holding the pelvis, lumbar spine, and knee in a flexed position until the hip reached a 90-degree flexion. Pressure changes were measured using a horizontally placed pressure biofeedback unit under the spine, near the posterior superior iliac spine. The test was repeated twice for each participant, and the average results were measured (Figure 2) [7].
Measurements were taken at three time points: baseline, the end of a six-week intervention, and after one month of follow-up. The primary outcome measured was pain intensity using a visual analog scale (VAS) ranging from 0-10. Secondary outcomes included lumbopelvic motor control, which was assessed using various tests, such as the knee lift abdominal test, bent knee fall-out test, waiter's bow test, sitting knee extension test, and transversus abdominis test. Acceptable reliability is demonstrated for this test battery[26, 27]. Further details about these outcome measures are presented in Table 1.
Pain Measurement: VAS measures the pain of patients subjectively. This scale is a 10-centimeter line, and patients are asked to grade their pain condition from 0 (no pain) to 10 (extreme amount of pain). The validity and reliability of this instrument have been reported to be very high [28].
Lumbopelvic Motor Control Measurement: The following tests were administered to assess lumbopelvic motor control, ensuring no order effects by randomization and incorporating one-minute breaks between each test. Participants completed three familiarization trials before each test.
Knee lifts abdominal test: The participant was lying on their back with their arms at their sides and feet on the floor. They were administered a test by gently raising their leg while holding the pelvis, lumbar spine, and knee in a flexed position until the hip reached a 90-degree flexion. Pressure changes were measured using a horizontally placed pressure biofeedback unit under the spine, near the posterior superior iliac spine. The test was repeated twice for each participant, and the average results were measured (Figure 2) [7].
A B
B 
 B
B 
C

Figure 2. Knee lifts abdominal test: (A) Position of the pressure biofeedback unit, (B) Start position for the test, and (C) Test movement |
Bent knee fall-out test: The participant was lying on their back with one hip flexed and the other leg fully extended. Two pressure biofeedback units were placed vertically under the lumbar spine. The units were inflated to a baseline pressure of 40 mm Hg. The participant performed two breathing cycles, and the pressure was then adjusted back to 40 mm Hg. They were instructed to maintain a neutral spine position while slowly rotating the extended leg outward by 45 degrees for a few seconds without moving the foot, pelvis, or lumbar spine. The maximum pressure deviation was recorded for analysis. This test was repeated twice for each participant, and the average was calculated [7].
Waiter bow test: Participants stood upright and were instructed to bend their trunk 50 degrees from the hip joint without any movement in the lumbar spine. The examiner visually assessed their ability to stabilize the trunk through isometric activity and maintain a neutral spine position. A score of one was given if the participant demonstrated trunk muscle activation and maintained a neutral spine position during the test. A score of zero was allocated if they were unable to do so. The test was repeated twice for each participant, and the average score was recorded [7].
Sitting knee extension test: Participants were seated with a neutral pelvic tilt. They were instructed to extend their knee while keeping their lumbar spine in a neutral position. The examiner visually assessed their ability to stabilize the trunk through isometric activity and maintain a neutral spine position. A score of one was given if the participant demonstrated trunk muscle activation and maintained a neutral spine position during knee extension. The test was repeated twice for each participant, and the average score was recorded [7].
Transversus abdominis test: Participants were positioned in a supine position with relaxed arms, feet flat on the floor, and knees bent at a 90-degree angle. The examiner assessed the contraction ability of the transversus abdominis muscle through observation and palpation. By placing their thumb around two centimeters inward and downward from the protrusion of the anterior superior iliac spine, the examiner asked participants to draw in their abdominal wall for 10 sec without moving their spine inward. A failed test, resulting in a zero score, was noted if there was spinal movement, bulging of the abdominal wall, inability to contract transversus abdominis muscle, or inability to sustain the contraction for ten seconds. A score of one was assigned if the contraction was maintained without spinal movement. The test was repeated twice for each participant, and the average score was recorded [7]. Reliability for assessing transversus abdominis recruitment by manual palpation is reported to be acceptable [26]. After conducting five tests, each patient's movement control score ranged from zero (failure in all five tests) to five (success in all five tests). The final motor control score was determined by calculating the mean score of the participants' motor control [29].
Exercise intervention
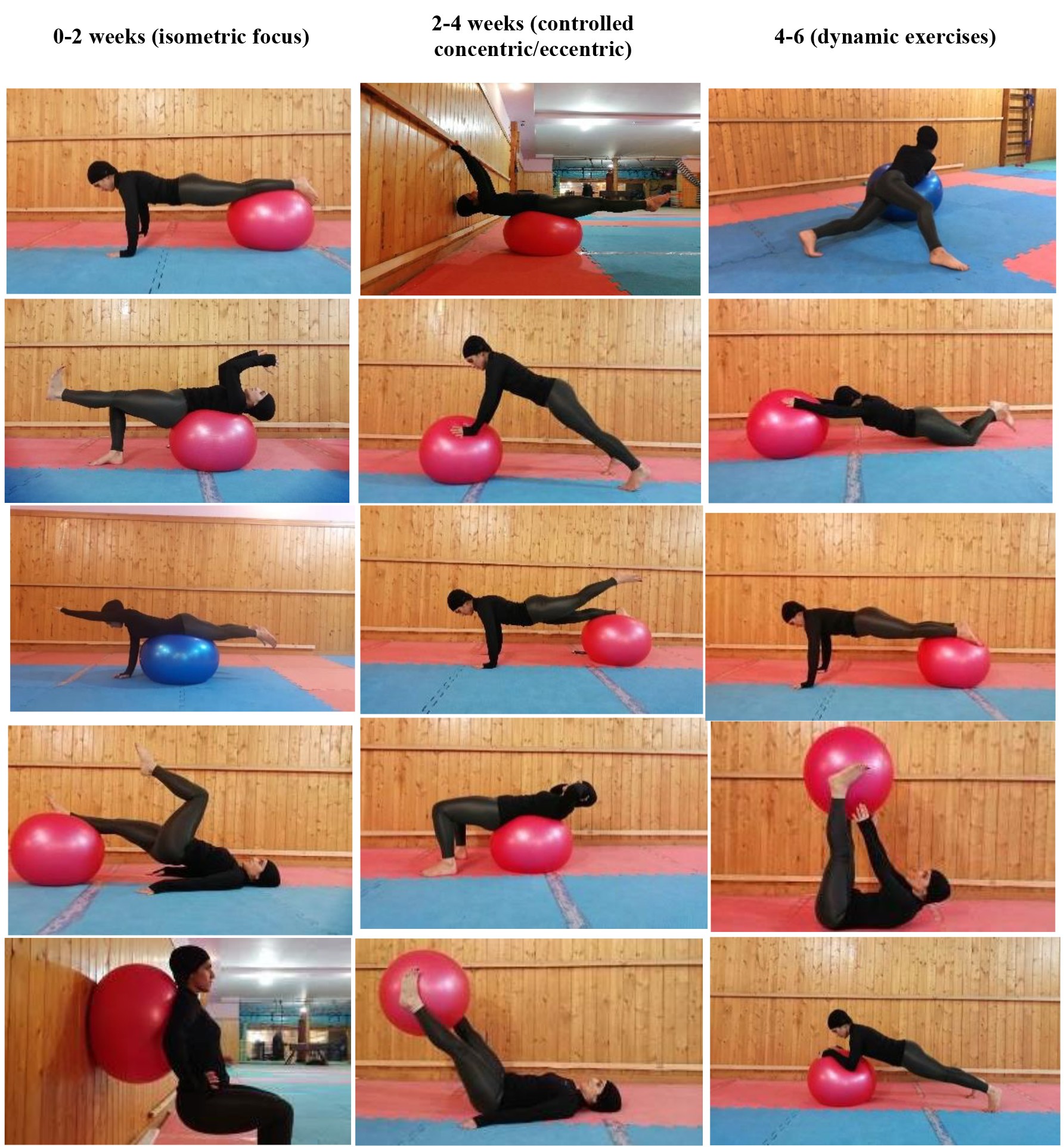
The experimental group underwent a six-week core
stability exercise program using a Swiss ball. The regimen consisted of three sessions per week, each lasting approximately 50 min. Each session began with a 10-minute warm-up, followed by 35-45 minutes of the main core stability exercise program. The sessions concluded with a five-minute cool-down, during which participants performed stretching movements. Participants performed each exercise for 10 sec, repeating it 10 times with 1-minute rest intervals between exercises. They were verbally and visually guided by a trained coach throughout the protocol in a group setting. On the contrary, the control group received routine physical therapy treatment, including transcutaneous electrical nerve stimulation and hot pack application over the painful area of the lower back, for 30 min, three days a week, for six consecutive weeks. Both groups were instructed to avoid engagement in other physical activities or training during the study period. The exercise protocol followed in this study was a modified version of the core stability exercises with a Swiss ball developed by Marshall et al. (2008) for patients with chronic LBP, tailored to fit the six-week duration [30]. In the experimental group, participants were required to attend a minimum of 15 out of 18 training sessions to remain part of the study. Detailed illustrations of the exercise program are illustrated in Figure 3.
Waiter bow test: Participants stood upright and were instructed to bend their trunk 50 degrees from the hip joint without any movement in the lumbar spine. The examiner visually assessed their ability to stabilize the trunk through isometric activity and maintain a neutral spine position. A score of one was given if the participant demonstrated trunk muscle activation and maintained a neutral spine position during the test. A score of zero was allocated if they were unable to do so. The test was repeated twice for each participant, and the average score was recorded [7].
Sitting knee extension test: Participants were seated with a neutral pelvic tilt. They were instructed to extend their knee while keeping their lumbar spine in a neutral position. The examiner visually assessed their ability to stabilize the trunk through isometric activity and maintain a neutral spine position. A score of one was given if the participant demonstrated trunk muscle activation and maintained a neutral spine position during knee extension. The test was repeated twice for each participant, and the average score was recorded [7].
Transversus abdominis test: Participants were positioned in a supine position with relaxed arms, feet flat on the floor, and knees bent at a 90-degree angle. The examiner assessed the contraction ability of the transversus abdominis muscle through observation and palpation. By placing their thumb around two centimeters inward and downward from the protrusion of the anterior superior iliac spine, the examiner asked participants to draw in their abdominal wall for 10 sec without moving their spine inward. A failed test, resulting in a zero score, was noted if there was spinal movement, bulging of the abdominal wall, inability to contract transversus abdominis muscle, or inability to sustain the contraction for ten seconds. A score of one was assigned if the contraction was maintained without spinal movement. The test was repeated twice for each participant, and the average score was recorded [7]. Reliability for assessing transversus abdominis recruitment by manual palpation is reported to be acceptable [26]. After conducting five tests, each patient's movement control score ranged from zero (failure in all five tests) to five (success in all five tests). The final motor control score was determined by calculating the mean score of the participants' motor control [29].
Exercise intervention
The experimental group underwent a six-week core
stability exercise program using a Swiss ball. The regimen consisted of three sessions per week, each lasting approximately 50 min. Each session began with a 10-minute warm-up, followed by 35-45 minutes of the main core stability exercise program. The sessions concluded with a five-minute cool-down, during which participants performed stretching movements. Participants performed each exercise for 10 sec, repeating it 10 times with 1-minute rest intervals between exercises. They were verbally and visually guided by a trained coach throughout the protocol in a group setting. On the contrary, the control group received routine physical therapy treatment, including transcutaneous electrical nerve stimulation and hot pack application over the painful area of the lower back, for 30 min, three days a week, for six consecutive weeks. Both groups were instructed to avoid engagement in other physical activities or training during the study period. The exercise protocol followed in this study was a modified version of the core stability exercises with a Swiss ball developed by Marshall et al. (2008) for patients with chronic LBP, tailored to fit the six-week duration [30]. In the experimental group, participants were required to attend a minimum of 15 out of 18 training sessions to remain part of the study. Detailed illustrations of the exercise program are illustrated in Figure 3.
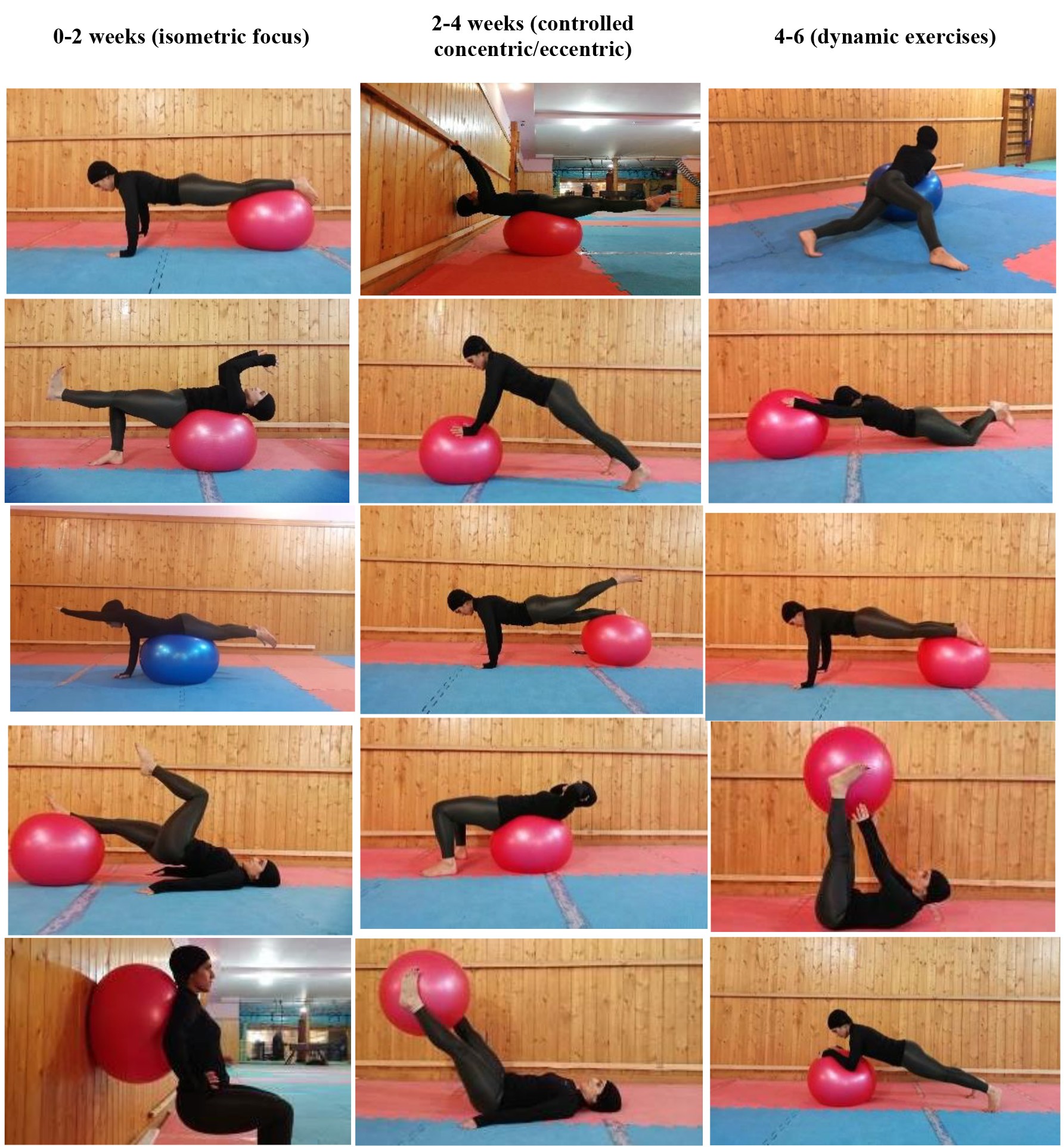
Figure 3. Swiss ball exercise program
Statistical analyses
The SPSS software (version 21) was used for data analysis. Results are expressed as means±SD. Kolmogorov-Smirnov testing was conducted to determine if the data were normally distributed. In normally distributed variables (all variables), mixed repeated measures ANOVA, repeated-measures ANOVA, Bonferroni post hoc test, and the independent samples Student's t-test were employed. The significance level was set at 0.05. In addition, Cohen's d effect sizes were calculated to measure the magnitude of the difference. The values of <.2, .21-.49, .50 to .79, and ≥ .80 are considered trivial, small, moderate, and large effects, respectively [31]. In addition, Eta-squared (η2) was used as a measure of effect size in the ANOVA (η2 around 0.01, 0.06, and 0.14 are considered small, medium, and large, respectively).
The SPSS software (version 21) was used for data analysis. Results are expressed as means±SD. Kolmogorov-Smirnov testing was conducted to determine if the data were normally distributed. In normally distributed variables (all variables), mixed repeated measures ANOVA, repeated-measures ANOVA, Bonferroni post hoc test, and the independent samples Student's t-test were employed. The significance level was set at 0.05. In addition, Cohen's d effect sizes were calculated to measure the magnitude of the difference. The values of <.2, .21-.49, .50 to .79, and ≥ .80 are considered trivial, small, moderate, and large effects, respectively [31]. In addition, Eta-squared (η2) was used as a measure of effect size in the ANOVA (η2 around 0.01, 0.06, and 0.14 are considered small, medium, and large, respectively).
Results
A total of 24 participants were recruited in this study. Table 1 summarizes the comparison of age, weight, height, and body mass index (BMI) between the experimental and control groups, including their means, standard deviations, and p-values. The mean scores of age, weight, height, and disability in experimental participants were reported as 43.08±5.10 years, 71.42±4.95 kg, 163.33±6.61 cm, and 51.41±7.82, respectively. Participants in the control group have an age of 41.08±8.71 years, weight of 73.17±4.89 kg, height of 160.91±5.96 cm, and disability of 53.66±4.90.
The group means for pain and motor control were measured at three time points: pre-test, post-test, and follow-up (Table 2). To analyze the data, a mixed repeated measures ANOVA (2*3) was used to examine within-group (pre-test, post-test, and follow-up) and between-group (experimental and control) factors. The results pointed to a significant interaction between group and time for pain and motor control variables (P< 0.001), as displayed in Table 2. Further analysis using independent t-tests revealed significant differences in pain values between the experimental and control groups at the post-test and follow-up (P<0.001). In addition, motor control values significantly differed between the two groups in the post-test (P<0.001) but not in the follow-up (P=0.055), as presented in Table 3.
The group means for pain and motor control were measured at three time points: pre-test, post-test, and follow-up (Table 2). To analyze the data, a mixed repeated measures ANOVA (2*3) was used to examine within-group (pre-test, post-test, and follow-up) and between-group (experimental and control) factors. The results pointed to a significant interaction between group and time for pain and motor control variables (P< 0.001), as displayed in Table 2. Further analysis using independent t-tests revealed significant differences in pain values between the experimental and control groups at the post-test and follow-up (P<0.001). In addition, motor control values significantly differed between the two groups in the post-test (P<0.001) but not in the follow-up (P=0.055), as presented in Table 3.
Table 1. Comparison of demographic characteristics and body mass index between experimental and control groups
| Variables | Experimental (n=12) | Control (n=12) | p-value |
| Age (year) | 43.1±5.1 | 41.1 ±8.7 | 0.78 |
| Weight (Kg) | 71.4±4.9 | 73.2±4.9 | 0.66 |
| High (Cm) | 163.3±6.6 | 160.9±5.9 | 0.86 |
| BMI (Kg/m2) | 26.8 ±2.84 | 28.3±2.81 | 0.69 |
Table 2. Group means of experimental and control groups at pre-test, post-test, and follow-up for pain and motor control
| Groups | Pre-test | Post-test | Follow-up | Time effects | Group effects | Interaction effects | |||||||
| f | p | Eta | f | p | Eta | f | p | Eta | |||||
| Pain (0-10 mm) |
Experimental | 49.73±4.68 | 32.24±6.45 | 34.36±5.58 | 46.5 | <.001 | 0.67 | 70.8 | <.001 | .76 | 34.5 | <.001 | .61 |
| Control | 51.25±2.56 | 50.35±3.57 | 49.43±2.87 | ||||||||||
| Motor Control (0-0 point) |
Experimental | 1.77±0.22 | 3.50±0.34 | 1.86±0.29 | 99.4 | <.001 | 0.81 | 120.51 | <.001 | .84 | 34.3 | <.001 | .61 |
| Control | 1.66±0.18 | 1.81±0.26 | 1.65±0.21 | ||||||||||
Table 3. Summary of independent t-test results
| Pre-test | Post-test | Follow-up | ||||||||||
| Mean Difference | t | p | Cohen's d | Mean Difference | t | p | Cohen's d | Mean Difference | t | p | Cohen's d | |
| Pain | 1.51 | .98 | .33 | .47 | 18.1* | 8.49 | <.001 | 3.70 | 15.07* | 8.31 | <.001 | 3.36 |
| Motor Control | .11 | 1.34 | .19 | .54 | 1.68* | 13.44 | <.001 | 5.58 | .21 | 2.02 | .055 | .82 |
* Significant difference (P<.01)
On the other hand, repeated-measures ANOVA results demonstrated that pain and motor control had significant differences between the pre-test, post-test, and follow-up phases in the experimental group (P<0.001). Therefore, the Bonferroni post-hoc test was utilized for separate comparisons (pre-test, post-test, and follow-up). The Bonferroni post-hoc test findings indicated significant differences between pre-test and post-test, and between pre-test and follow-up for pain values (P< 0.001). However, the difference between post-test and follow-up was not statistically significant (P=0.172) (Table 4).
Table 4. Summary of the repeated-measures ANOVA and the Bonferroni posthoc test results for pain and motor control in pre-test, post-test, and follow-up
| F | p | Mean Difference | p | Cohen's d | ||
| Pain | 56.21 | <.001 | Pre-test – post-test | 17.48* | <.001 | 3.31 |
| Pre-test – follow-up | 15.37* | <.001 | 2.98 | |||
| Post-test – follow-up | 2.11 | .172 | .55 | |||
| Motor Control | 141.66 | <.001 | Pre-test – post-test | 1.72* | <.001 | 6.04 |
| Pre-test – follow-up | .09 | 1.00 | .34 | |||
| Post-test – follow-up | 1.63* | <.001 | 5.19 | |||
* Significant difference (P<.01).
Discussion
This study is one of the few investigating the impact of Swiss ball core stabilization on pain and motor control in individuals with nonspecific chronic LBP. The findings demonstrated a significant reduction in pain intensity after core stability exercises on a Swiss ball, and the benefits persist during follow-up. Other studies comparing core stabilization programs with routine physical therapy or Pilates exercises also support the positive effects on muscle activity, thickness, pain, and disability in chronic LBP patients, indicating the potential efficacy of these interventions[32, 33].
The present study revealed a significant difference in motor control between the two groups following core stability exercises, though this effect was not sustained one month post-intervention. Consistent with these findings, Eliks et al. (2019) observed that Pilates-based exercises can enhance motor control quality in chronic nonspecific LBP [18]. Wang et al. (2023) compared postural control and core stability exercises in chronic LBP patients, reporting that both protocols induced balance improvements potentially linked to enhanced motor control of deep trunk muscles[20]. Park et al. (2016) and Mendis et al. (2016) corroborated that motor control exercises in the lumbopelvic region could improve muscle recruitment patterns and motor control, aligning with the results of the present study [19, 21]. On the contrary, Boucher et al. (2016) reported that stabilizing exercises in their study failed to achieve sensory-rich improvement in LBP patients [23], suggesting that the exercises employed were not specifically designed to enhance lumbar proprioception.
Core stability exercises enhance motor control in the lumbopelvic region through targeted engagement of muscles responsible for spinal and pelvic stability, promoting increased strength and endurance[19]. These exercises focus on key muscles, such as transversus abdominis and multifidus, addressing imbalances commonly associated with such conditions as LBP [34]. By specifically activating these muscles, core stability exercises improve neuromuscular control and counteract abnormal muscle activity patterns seen in LBP, where mobilizing muscles, such as abdominal muscles, are overactive, while stabilizing muscles, such as multifidus, are underactive [34]. The exercises work to reverse selective atrophy, particularly in type II muscle fibers of multifidus, ultimately improving muscle fiber size [35, 36]. This reversal process helps restore balance between agonist and stabilizing muscles[37], leading to more coordinated movement patterns and, consequently, enhanced motor control in the lumbopelvic region. In addition, these exercises contribute to proprioceptive development, heightening the body's awareness of its position and movement [20]. This increased proprioception can result in more precise and controlled movements in the lumbopelvic region. Overall, the emphasis on core stability leads to improved muscle recruitment patterns, enhanced stability, and superior motor control, offering therapeutic benefits for individuals with LBP [32].
Core stability exercises have been demonstrated to effectively enhance neuromuscular control mechanisms in individuals with nonspecific chronic low back pain, potentially by improving sensory and motor control of the trunk and core muscles[38]. These exercises not only contribute to the development of trunk stability but also reduce injuries to the spine, leading to a decrease in pain[39]. In addition, core stability exercises appear to correct postural asymmetry, minimizing damage from uneven pressure on joints and intervertebral discs[5]. A study suggests that motor control disorders in the lumbopelvic region stemming from electromyographic activity disturbances in trunk muscles, such as the transversus abdominis and multifidus, could be a significant factor in triggering low back pain[7].
Improved motor control in this study may be ascribed to the alleviation of pain in patients, as pain can adversely affect lumbar motor control through alterations in muscle recruitment, impaired balance control, and proprioception[40]. Core stability exercises likely contribute to pain reduction and subsequent improvements in motor control patterns in the lumbar region by enhancing stability, improving trunk muscle activity, and optimizing neuromuscular control[41]. However, further confirmation through electromyography or imaging studies is warranted. Despite these positive effects, motor control declined in the one-month follow-up, potentially due to the short duration of the exercise program, which may not have induced long-term adaptations. Notably, there is a lack of existing studies investigating the sustained impact of core exercises on motor control gains in chronic LBP. Previous studies suggest that low abdominal muscle strength is a contributing factor to LBP, and core stability exercises can address this issue by enhancing the volume and strength of trunk muscles[42, 43]. Furthermore, exercises may improve the activity and rhythm of core muscles in the lumbopelvic region; moreover, they can address dysfunction in deep trunk muscles, providing an effective strategy for alleviating chronic LBP[44, 45].
Stability exercises with Swiss balls offer considerable advantages over routine stability exercises due to their increased instability level. This dynamic surface requires greater muscle activation, potentially enhancing neuromuscular coordination and proprioception[13, 22]. Swiss ball exercises also allow for a more extensive range of motion, leading to more comprehensive muscle recruitment and engagement[19]. These exercises can result in more significant functional gains, improved core strength, and enhanced balance, making them valuable in rehabilitation programs for individuals recovering from low back pain or seeking injury prevention[32, 36]. In addition, Swiss ball exercises offer versatility and customization options to meet specific patient needs and abilities[17].
As evidenced by the results of our study, the practical implications of stability exercises with Swiss balls are wide-ranging. They can be used in clinical practice for rehabilitation, athletic training for injury prevention and performance enhancement, and preventive care settings. Individuals can also incorporate them into home exercise routines for long-term management of low back pain and overall fitness. Further research and education are necessary to optimize their use and ensure safe implementation across various settings.
The present study is subject to several limitations that could impact the robustness of its findings. Firstly, the small sample size may compromise the generalizability of the results. Furthermore, the relatively brief duration
of the exercise protocol might contribute to temporary and non-sustainable changes in motor control. Other limitations related to uncontrolled variables, such as sitting time, occupation, and sitting style, suggest that these results should be interpreted with great caution. Future research that accounts for these factors is necessary to validate and extend our findings. Another constraint is the absence of electromyography (EMG) or imaging methods, which, due to their cost, could hinder the establishment of a significant correlation between the findings and muscle activity or morphology.
This study is one of the few investigating the impact of Swiss ball core stabilization on pain and motor control in individuals with nonspecific chronic LBP. The findings demonstrated a significant reduction in pain intensity after core stability exercises on a Swiss ball, and the benefits persist during follow-up. Other studies comparing core stabilization programs with routine physical therapy or Pilates exercises also support the positive effects on muscle activity, thickness, pain, and disability in chronic LBP patients, indicating the potential efficacy of these interventions[32, 33].
The present study revealed a significant difference in motor control between the two groups following core stability exercises, though this effect was not sustained one month post-intervention. Consistent with these findings, Eliks et al. (2019) observed that Pilates-based exercises can enhance motor control quality in chronic nonspecific LBP [18]. Wang et al. (2023) compared postural control and core stability exercises in chronic LBP patients, reporting that both protocols induced balance improvements potentially linked to enhanced motor control of deep trunk muscles[20]. Park et al. (2016) and Mendis et al. (2016) corroborated that motor control exercises in the lumbopelvic region could improve muscle recruitment patterns and motor control, aligning with the results of the present study [19, 21]. On the contrary, Boucher et al. (2016) reported that stabilizing exercises in their study failed to achieve sensory-rich improvement in LBP patients [23], suggesting that the exercises employed were not specifically designed to enhance lumbar proprioception.
Core stability exercises enhance motor control in the lumbopelvic region through targeted engagement of muscles responsible for spinal and pelvic stability, promoting increased strength and endurance[19]. These exercises focus on key muscles, such as transversus abdominis and multifidus, addressing imbalances commonly associated with such conditions as LBP [34]. By specifically activating these muscles, core stability exercises improve neuromuscular control and counteract abnormal muscle activity patterns seen in LBP, where mobilizing muscles, such as abdominal muscles, are overactive, while stabilizing muscles, such as multifidus, are underactive [34]. The exercises work to reverse selective atrophy, particularly in type II muscle fibers of multifidus, ultimately improving muscle fiber size [35, 36]. This reversal process helps restore balance between agonist and stabilizing muscles[37], leading to more coordinated movement patterns and, consequently, enhanced motor control in the lumbopelvic region. In addition, these exercises contribute to proprioceptive development, heightening the body's awareness of its position and movement [20]. This increased proprioception can result in more precise and controlled movements in the lumbopelvic region. Overall, the emphasis on core stability leads to improved muscle recruitment patterns, enhanced stability, and superior motor control, offering therapeutic benefits for individuals with LBP [32].
Core stability exercises have been demonstrated to effectively enhance neuromuscular control mechanisms in individuals with nonspecific chronic low back pain, potentially by improving sensory and motor control of the trunk and core muscles[38]. These exercises not only contribute to the development of trunk stability but also reduce injuries to the spine, leading to a decrease in pain[39]. In addition, core stability exercises appear to correct postural asymmetry, minimizing damage from uneven pressure on joints and intervertebral discs[5]. A study suggests that motor control disorders in the lumbopelvic region stemming from electromyographic activity disturbances in trunk muscles, such as the transversus abdominis and multifidus, could be a significant factor in triggering low back pain[7].
Improved motor control in this study may be ascribed to the alleviation of pain in patients, as pain can adversely affect lumbar motor control through alterations in muscle recruitment, impaired balance control, and proprioception[40]. Core stability exercises likely contribute to pain reduction and subsequent improvements in motor control patterns in the lumbar region by enhancing stability, improving trunk muscle activity, and optimizing neuromuscular control[41]. However, further confirmation through electromyography or imaging studies is warranted. Despite these positive effects, motor control declined in the one-month follow-up, potentially due to the short duration of the exercise program, which may not have induced long-term adaptations. Notably, there is a lack of existing studies investigating the sustained impact of core exercises on motor control gains in chronic LBP. Previous studies suggest that low abdominal muscle strength is a contributing factor to LBP, and core stability exercises can address this issue by enhancing the volume and strength of trunk muscles[42, 43]. Furthermore, exercises may improve the activity and rhythm of core muscles in the lumbopelvic region; moreover, they can address dysfunction in deep trunk muscles, providing an effective strategy for alleviating chronic LBP[44, 45].
Stability exercises with Swiss balls offer considerable advantages over routine stability exercises due to their increased instability level. This dynamic surface requires greater muscle activation, potentially enhancing neuromuscular coordination and proprioception[13, 22]. Swiss ball exercises also allow for a more extensive range of motion, leading to more comprehensive muscle recruitment and engagement[19]. These exercises can result in more significant functional gains, improved core strength, and enhanced balance, making them valuable in rehabilitation programs for individuals recovering from low back pain or seeking injury prevention[32, 36]. In addition, Swiss ball exercises offer versatility and customization options to meet specific patient needs and abilities[17].
As evidenced by the results of our study, the practical implications of stability exercises with Swiss balls are wide-ranging. They can be used in clinical practice for rehabilitation, athletic training for injury prevention and performance enhancement, and preventive care settings. Individuals can also incorporate them into home exercise routines for long-term management of low back pain and overall fitness. Further research and education are necessary to optimize their use and ensure safe implementation across various settings.
The present study is subject to several limitations that could impact the robustness of its findings. Firstly, the small sample size may compromise the generalizability of the results. Furthermore, the relatively brief duration
of the exercise protocol might contribute to temporary and non-sustainable changes in motor control. Other limitations related to uncontrolled variables, such as sitting time, occupation, and sitting style, suggest that these results should be interpreted with great caution. Future research that accounts for these factors is necessary to validate and extend our findings. Another constraint is the absence of electromyography (EMG) or imaging methods, which, due to their cost, could hinder the establishment of a significant correlation between the findings and muscle activity or morphology.
Conclusion
A six-week core stabilization program on a Swiss ball demonstrated a significant positive impact on reducing pain intensity and enhancing motor control in individuals with nonspecific chronic LBP when compared to routine physical therapy. While the effects on pain intensity persisted during the one-month follow-up, improvements in motor control were not sustained. This outcome highlights the need for additional time-series studies or investigations involving subgroups undergoing different treatment modalities to explore these findings further and understand them.
Ethical Considerations
Compliance with ethical guidelines
This study obtained approval from the Ethics Committee of the Sport Sciences Research Institute (Ethics number: IR.SSRC.REC.1399.076), and all participants provided informed consent.
Funding
This study was a part of the master's thesis in animal physiology and was carried out with the financial support of the Shafagh Institute of Higher Education.
Authors' contributions
All authors contributed equally to this article.
Conflicts of interest
The authors have no conflict of interest.
Acknowledgments
The authors express their gratitude to the staff of the Shafagh Institute of Higher Education and all participants for their cooperation and assistance in conducting this study.
References
- Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: a systematic review and meta-analysis. Spine J. 2014;14(10):2299-319. [DOI: 10.1016/j.spinee.2014.01.026][PMID]
- Meucci RD, Fassa AG, Faria NMX. Prevalence of chronic low back pain: systematic review. Rev Saude Publica. 2015;49:1. [DOI: 10.1590/S0034-8910.2015049005874] [PMID] [PMCID]
- Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968-74. [DOI: 10.1136/annrheumdis-2013-204428] [PMID]
- da Silva RA, Vieira ER, Fernandes KBP, Andraus RA, Oliveira MR, Sturion LA, et al. People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil Rehabil. 2018;40(11):1294-300. [DOI: 10.1080/09638288.2017.1294627] [PMID]
- Pereira LM, Obara K, Dias JM, Menacho MO, Guariglia DA, Schiavoni D, et al. Comparing the Pilates method with no exercise or lumbar stabilization for pain and functionality in patients with chronic low back pain: systematic review and meta-analysis. Clin Rehabil. 2012;26(1):10-20. [DOI: 10.1177/0269215511411113] [PMID]
- Madigan ML, Davidson BS, Nussbaum MA. Postural sway and joint kinematics during quiet standing are affected by lumbar extensor fatigue. Hum Mov Sci. 2006;25(6):788-99. [DOI: 10.1016/j.humov.2006.04.004] [PMID]
- Grosdent S, Demoulin C, Rodriguez de La Cruz C, Giop R, Tomasella M, Crielaard JM, et al. Lumbopelvic motor control and low back pain in elite soccer players: a cross-sectional study. J Sports Sci. 2016;34(11):1021-9. [DOI: 10.1080/02640414.2015.1085077] [PMID]
- Fatoye F, Gebrye T, Ryan CG, Useh U, Mbada C. Global and regional estimates of clinical and economic burden of low back pain in high-income countries: a systematic review and meta-analysis. Front Public Health. 2023;11:1098100. [DOI: 10.3389/fpubh.2023.1098100] [PMID] [PMCID]
- Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. 2021;9(9):CD009790. [DOI: 10.1002/14651858.CD009790.pub2] [PMID] [PMCID]
- Macedo LG, Hodges PW, Bostick G, Hancock M, Laberge M, Hanna S, et al. Which Exercise for Low Back Pain? (WELBack) trial predicting response to exercise treatments for patients with low back pain: a validation randomised controlled trial protocol. BMJ Open. 2021;11(1):e042792. [DOI: 10.1136/bmjopen-2020-042792] [PMID] [PMCID]
- Alikhajeh Y, Barabadi E, Mohammad Rahimi GR. A Comparison of 6 Weeks of Aquatic Exercise and Kinesio Taping in Patients With Chronic Nonspecific Low Back Pain. J Sport Rehabil. 2020;30(1):37-42. [DOI: 10.1123/jsr.2019-0185] [PMID]
- Hides J, Stanton W, Mendis MD, Sexton M. The relationship of transversus abdominis and lumbar multifidus clinical muscle tests in patients with chronic low back pain. Man Ther. 2011;16(6):573-7. [DOI: 10.1016/j.math.2011.05.007] [PMID]
- Hides JA, Stanton WR, Mendis MD, Gildea J, Sexton MJ. Effect of motor control training on muscle size and football games missed from injury. Med Sci Sports Exerc. 2012;44(6):1141-9. [DOI: 10.1249/MSS.0b013e318244a321] [PMID]
- Gomes-Neto M, Lopes JM, Conceição CS, Araujo A, Brasileiro A, Sousa C, et al. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis. Phys Ther Sport. 2017;23:136-42. [DOI: 10.1016/j.ptsp.2016.08.004] [PMID]
- Smith BE, Littlewood C, May S. An update of stabilisation exercises for low back pain: a systematic review with meta-analysis. BMC Musculoskelet Disord. 2014;15:416. [DOI: 10.1186/1471-2474-15-416] [PMID] [PMCID]
- Stuge B. Evidence of stabilizing exercises for low back- and pelvic girdle pain – a critical review. Braz J Phys Ther. 2019;23(2):181-6. [DOI: 10.1016/j.bjpt.2018.11.006] [PMID] [PMCID]
- Young KJ, Je CW, Hwa ST. Effect of proprioceptive neuromuscular facilitation integration pattern and swiss ball training on pain and balance in elderly patients with chronic back pain. J Phys Ther Sci. 2015;27(10):3237-40. [DOI: 10.1589/jpts.27.3237] [PMID] [PMCID]
- Eliks M, Zgorzalewicz-Stachowiak M, Zenczak-Praga K. Application of Pilates-based exercises in the treatment of chronic nonspecific low back pain: state of the art. Postgrad Med J. 2019;95(1119):41-5. [DOI: 10.1136/postgradmedj-2018-135920] [PMID] [PMCID]
- Mendis MD, Hides JA. Effect of motor control training on hip muscles in elite football players with and without low back pain. J Sci Med Sport. 2016;19(11):866-71. [DOI: 10.1016/j.jsams.2016.02.008] [PMID]
- Wang H, Fan Z, Liu X, Zheng J, Zhang S, Zhang S, et al. Effect of Progressive Postural Control Exercise Versus Core Stability Exercise in Young Adults with Chronic Low Back Pain: A Randomized Controlled Trial. Pain Ther. 2023;12(1):293-308. [DOI: 10.1007/s40122-022-00458-x] [PMID] [PMCID]
- Park KN, Kwon OY, Yi CH, Cynn HS, Weon JH, Kim TH, et al. Effects of Motor Control Exercise Vs Muscle Stretching Exercise on Reducing Compensatory Lumbopelvic Motions and Low Back Pain: A Randomized Trial. J Manipulative Physiol Ther. 2016;39(8):576-85. [DOI: 10.1016/j.jmpt.2016.07.006] [PMID]
- Chung S, Lee J, Yoon J. Effects of stabilization exercise using a ball on mutifidus cross-sectional area in patients with chronic low back pain. J Sports Sci Med. 2013;12(3):533-41. [PMID] [PMCID]
- Boucher JA, Preuss R, Henry SM, Dumas JP, Larivière C. The effects of an 8-week stabilization exercise program on lumbar movement sense in patients with low back pain. BMC Musculoskelet Disord. 2016;17:23. [DOI: 10.1186/s12891-016-0875-4] [PMID] [PMCID]
- Amundsen PA, Evans DW, Rajendran D, Bright P, Bjørkli T, Eldridge S, et al. Inclusion and exclusion criteria used in nonspecific low back pain trials: a review of randomised controlled trials published between 2006 and 2012. BMC Musculoskelet Disord. 2018;19(1):113. [DOI: 10.1186/s12891-018-2034-6] [PMID] [PMCID]
- Otadi K, Nakhostin Ansari N, Sharify S, Fakhari Z, Sarafraz H, Aria A, et al. Effects of combining diaphragm training with electrical stimulation on pain, function, and balance in athletes with chronic low back pain: a randomized clinical trial. BMC Sports Sci Med Rehabil. 2021;13(1):20. [DOI: 10.1186/s13102-021-00250-y] [PMID] [PMCID]
- Pena Costa LO, Menezes Costa LC, Cançado RL, De Melo Oliveira W, Ferreira PH. Intra-tester reliability of two clinical tests of transversus abdominis muscle recruitment. Physiother Res Int. 2006;11(1):48-50. [DOI: 10.1002/pri.39] [PMID]
- Denteneer L, Stassijns G, De Hertogh W, Truijen S, Van Daele U. Inter-and intrarater reliability of clinical tests associated with functional lumbar segmental instability and motor control impairment in patients with low back pain: a systematic review. Arch Phys Med Rehabil. 2017;98(1):151-164.e6. [DOI: 10.1016/j.apmr.2016.07.020] [PMID]
- Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8(12):1153-7. [DOI: 10.1111/j.1553-2712.2001.tb01132.x] [PMID]
- Luomajoki H, Kool J, De Bruin ED, Airaksinen O. Movement control tests of the low back; evaluation of the difference between patients with low back pain and healthy controls. BMC Musculoskelet Disord. 2008;9:170. [DOI: 10.1186/1471-2474-9-170] [PMID] [PMCID]
- Marshall PW, Murphy BA. Muscle activation changes after exercise rehabilitation for chronic low back pain. Arch Phys Med Rehabil. 2008;89(7):1305-13. [DOI: 10.1016/j.apmr.2007.11.051] [PMID]
- Cohen J. Eta-Squared and Partial Eta-Squared in Fixed Factor Anova Designs. Educational and Psychological Measurement. 1973;33(1):107-12. [DOI: 10.1177/001316447303300111]
- Narouei S, Barati Ah, Akuzawa H, Talebian S, Ghiasi F, Akbari A, et al. Effects of core stabilization exercises on thickness and activity of trunk and hip muscles in subjects with nonspecific chronic low back pain. J Bodyw Mov Ther. 2020;24(4):138-46. [DOI: 10.1016/j.jbmt.2020.06.026] [PMID]
- Alves MC, de Souza Neto RJ, Barbosa RI, Marcolino AM, Kuriki HU. Effects of a Pilates protocol in individuals with nonspecific low back pain compared with healthy individuals: Clinical and electromyographic analysis. Clin Biomech (Bristol, Avon). 2020;72:172-8. [DOI: 10.1016/j.clinbiomech.2019.12.009] [PMID]
- Ng JKF, Richardson CA, Parnianpour M, Kippers V. EMG activity of trunk muscles and torque output during isometric axial rotation exertion: a comparison between back pain patients and matched controls. J Orthop Res. 2002;20(1):112-21. [DOI: 10.1016/S0736-0266(01)00067-5] [PMID]
- Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, Bourgois J, Dankaerts W, et al. Effects of three different training modalities on the cross sectional area of the lumbar multifidus muscle in patients with chronic low back pain. Br J Sports Med. 2001;35(3):186-91. [DOI: 10.1136/bjsm.35.3.186] [PMID] [PMCID]
- liziene I, Sipaviciene S, Klizas S, Imbrasiene D. Effects of core stability exercises on multifidus muscles in healthy women and women with chronic low-back pain. J Back Musculoskelet Rehabil. 2015;28(4):841-7. [DOI: 10.3233/BMR-150596] [PMID]
- Gringmuth RH, Jackson C. Therapeutic exercise for spinal segmental stabilization in low back pain: scientific basis and clinical approach. J Can Chiropr Assoc. 2000;44(2):125. [PMCID]
- Wallwork TL, Stanton WR, Freke M, Hides JA. The effect of chronic low back pain on size and contraction of the lumbar multifidus muscle. Man Ther. 2009;14(5):496-500. [DOI: 10.1016/j.math.2008.09.006] [PMID]
- Posadzki P, Lizis P, Hagner-Derengowska M. Pilates for low back pain: a systematic review. Complement Ther Clin Pract. 2011;17(2):85-9. [DOI: 10.1016/j.ctcp.2010.09.005] [PMID]
- Meier ML, Vrana A, Schweinhardt P. Low Back Pain: The Potential Contribution of Supraspinal Motor Control and Proprioception. Neuroscientist. 2019;25(6):583-96. [DOI: 10.1177/1073858418809074] [PMID] [PMCID]
- Takala E-P, Viikari-Juntura E. Do functional tests predict low back pain? Spine (Phila Pa 1976). 2000;25(16):2126-32. [DOI: 10.1097/00007632-200008150-00018] [PMID]
- Guclu-Gunduz A, Citaker S, Irkec C, Nazliel B, Batur-Caglayan HZ. The effects of pilates on balance, mobility and strength in patients with multiple sclerosis. NeuroRehabilitation. 2014;34(2):337-42. [DOI: 10.3233/NRE-130957] [PMID]
- ee JS, Yang SH, Koog YH, Jun HJ, Kim SH, Kim KJ. Effectiveness of sling exercise for chronic low back pain: a systematic review. J Phys Ther Sci. 2014;26(8):1301-6. [DOI: 10.1589/jpts.26.1301] [PMID] [PMCID]
- Ferreira PH, Ferreira ML, Hodges PW. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine (Phila Pa 1976). 2004;29(22):2560-6. [DOI: 10.1097/01.brs.0000144410.89182.f9] [PMID]
- Macedo LG, Saragiotto BT, Yamato TP, Costa LO, Menezes Costa LC, Ostelo RW, et al. Motor control exercise for acute nonspecific low back pain. Cochrane Database Syst Rev. 2016;2(2):CD012085. [DOI: 10.1002/14651858.CD012085] [PMID] [PMCID]
Type of Study: Original |
Subject:
Orthopedics and Biomechanics
Received: 2023/11/13 | Accepted: 2024/07/31 | Published: 2023/03/10
Received: 2023/11/13 | Accepted: 2024/07/31 | Published: 2023/03/10
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |